Abstract
Sickle Cell Disease (SCD) is a genetic disorder in which sudden onset of painful vaso-occlusive crises (VOC) can occur due to the obstruction of the microvasculature by the rigid sickled red blood cells. We have previously shown that pain itself could be a trigger for VOC by causing significant neural mediated vasoconstriction in the microvasculature and thereby promoting obstruction and eventual progression to VOC. Many scientific models and experimental studies have shown that increased attention to painful stimuli influences subjective pain measures such as pain sensitivity and tolerance and can alter acute pain outcomes. In this study, we explored the role of pain attention in modulating the objective vasoconstriction response to thermal pain in SCD and controls.
Methods: 76 subjects were exposed to heat pain via a TSA II Neurosensory analyzer thermode that was placed on the arm and microvascular blood flow (MBF) was measured in the contralateral thumb using photo-plethysmography (PPG). In the first cohort consisting of 23 SCD and 25 controls, subjects were alerted of upcoming heat pain and they were required to focus on the stimuli and respond when they reached their threshold for heat pain. In the second cohort consisting of 17 SCD and 11 controls, subjects were exposed to their predetermined specific heat pain threshold temperature without alerting them or calling any attention to the pain stimuli.
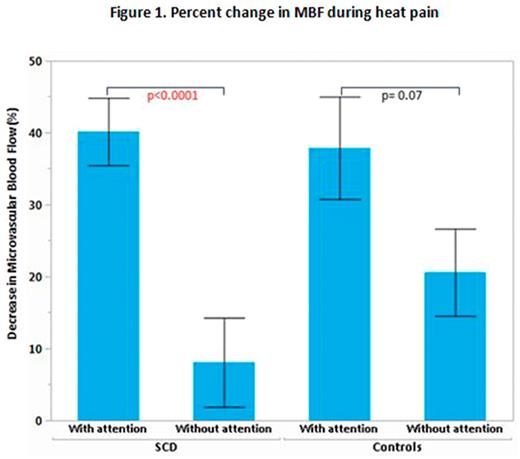
We derived the mean MBF during heat pain from the PPG amplitude and calculated the percent change in MBF from the baseline period immediately prior to the pain. Higher percent change signifies stronger vasoconstriction.
Results: There was a significant drop in MBF during heat pain in both cohorts but the percent change in MBF was higher in the cohort with pain attention (p<0.0001). Among SCD subjects, those with pain attention had a significantly higher percent change in MBF than those without pain attention (p<0.0001). This effect was only seen to a lesser degree among controls (Figure 1). The average heat pain threshold was lower (43.5 °C) in the cohort with pain attention compared to the cohort without pain attention (47.4 °C) (p<0.0001). This suggests that along with higher subjective pain sensitivity, there is greater drop in MBF due to pain attention.
Conclusions: Attention to painful stimuli significantly modulates the neural mediated vasoconstriction response to thermal pain in SCD but not so in controls. These data suggest that SCD subjects have significant pain anxiety likely from previous pain experiences and this might contribute to progressive vaso-occlusion by enhancing their vasoconstriction response to pain. Attenuation of this pain anxiety response in the peripheral perfusion might be a potential modality by which cognitive behavior therapies could improve pain outcomes in SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal